In a Nutshell:
- More than a decade after Medicaid was expanded under the Affordable Care Act, Michigan’s Medicaid expansion is going strong
- Availability of Medicaid coverage helped ensure people could access needed healthcare during the coronavirus pandemic
- With broad economic and social benefits, the Healthy Michigan Plan continues to pay dividends for Michigan residents, whether or not they are enrolled in the program
In our 2017 report analyzing the Healthy Michigan Plan, the Research Council found that Medicaid expansion was not only an efficient and effective way to increase the number of individuals with health insurance coverage, but also provided broad economic and social benefits to the entire state.
At the time we authored this report, Medicaid expansion remained a controversial policy, with only half of the states adopting expansion under the Affordable Care Act, and an additional seven states expanding their Medicaid programs through Section 1115 Demonstration Waivers (allowing flexibility for experimental, state-specific approaches to Medicaid policy and service delivery).
Michigan’s Experience
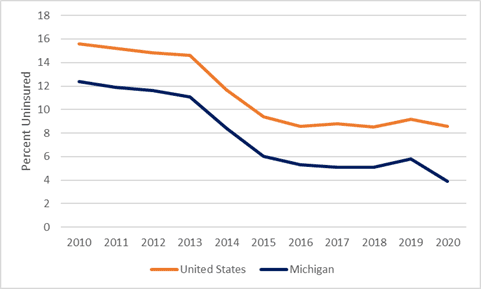
Implementation of Healthy Michigan began in April 2014. Due to pent up demand, enrollment surpassed the first-year goal of 322,000 enrollees in just 100 days and has contributed to a large drop in the number of uninsured in Michigan.
Proportion of the Population Lacking Health Insurance, U.S. and Michigan, 2010-2020
Today, 985,862 Michiganders receive health insurance through the Healthy Michigan Plan. A sizeable proportion of beneficiaries are young (18-34 years of age), and most work in low wage or seasonal jobs that do not provide insurance.
But, beyond these numbers, what has Medicaid expansion meant for health care cost, access, and quality in Michigan?
By effectively managing care and preventing overcharging by providers, the per-person cost of Medicaid plans has grown much more slowly than the cost of employer-sponsored health plans during the same period. Moreover, research suggests that people in states that expanded Medicaid pay less for non-Medicaid private health plans as a result. Private health plans are less expensive in these states because Medicaid expansion leads to a healthier individual market risk pool and a reduction of bad debt on the part of health providers, among many other factors.
As for the costs incurred by direct beneficiaries of the program, Michigan obtained a federal waiver to include copays and premium contributions for Medicaid enrollees; these costs are capped at a percentage of income and have remained affordable for the people who pay them.
An insurance policy alone doesn’t guarantee access, of course. Yet, despite fears that more insured individuals would overcrowd medical offices, Medicaid expansion did not have a negative effect on primary care appointment availability for new Medicaid patients in Michigan. Access to behavioral health and dental services remains challenging in Michigan and elsewhere. (Moreover, with our maldistribution of health care providers, access in some parts of the state are a challenge no matter the source of insurance). Yet in terms of access, Medicaid beneficiaries fare as well as (and in some cases, better than) people with employer-sponsored health insurance plans.
And what of quality?
Medicaid beneficiaries generally receive high-quality care. In fact, the Healthy Michigan Plan has facilitated health improvement for many enrollees. Evidence from before the pandemic suggested that this improved health facilitates greater workforce participation, better performance at school or work, and greater financial stability. Every person in Michigan enjoys a portion of these benefits, whether or not people are themselves enrolled in Medicaid; indeed, the substantial economic benefits that the state has enjoyed from Medicaid expansion have been spread very broadly.
Current Status of State Medicaid Expansions
Evidence of success from states like Michigan that adopted Medicaid expansion early in proximity to passage of the Affordable Care Act has been hard to ignore. Today, 39 states have expanded their Medicaid programs, and others remain poised to do so. This fact, combined with the 2021 Supreme Court Decision to uphold the Affordable Care Act, suggests that Medicaid expansion is now firmly entrenched in federal and state health policy.
Medicaid Enrollment Surged During COVID-19 Pandemic
While the social and economic benefits of state Medicaid programs have been well-established, the coronavirus pandemic of 2020 has made clear Medicaid’s value as a core safety net program.
Since February 2020, enrollment in Medicaid and the Children’s Health Insurance Program (CHIP) grew precipitously. This is partly due to economic downturns and the loss of both income and health insurance associated with employment, leading to larger numbers of Medicaid-eligible individuals. It may also be that income loss, rather than job loss, has contributed to increased eligibility. Additionally, provisions in the federal Families First Coronavirus Response Act (FFCRA) required states to ensure continuous coverage for Medicaid enrollees using an enhanced federal matching rate as a financial incentive to do so during the public health emergency.
In Michigan, the number of average total monthly Medicaid beneficiaries grew from 2,672,074 in 2020 to 3,102,622 so far in 2022, a 16 percent increase. The increase was driven by a rise in average monthly Healthy Michigan enrollment, from 720,892 enrollees in 2020 to 969,865 enrollees in 2022. Yet, Michigan’s Medicaid enrollment increase falls below the national average and is dwarfed by many other states like Utah, Nebraska, Missouri, and Florida.
Increased enrollment may have been attenuated in Michigan for a variety of reasons. Compared to Florida, one of the top five states for uninsured residents at the pandemic’s onset, Michigan entered the pandemic with an expanded Medicaid program and a smaller percentage of its residents uninsured. Unlike Utah, Nebraska, or Missouri, Michigan’s Medicaid expansion is well established and intertwined with other health insurance coverage options, creating a higher baseline coverage with less room for growth. It may also be that Michigan’s relatively aged population (ranking eighth nationally for the number of Medicare beneficiaries) was more insulated from pandemic-related insurance or income loss. State policies to address the pandemic may have played a role in this insulation as well.
Regardless of the relative level of state growth, Michigan and other states face a challenge as the federal pandemic state of emergency ends. Medicaid recertification will resume and may eliminate health insurance benefits for as many as 15 million Americans. Some may no longer be eligible or need Medicaid coverage; in other cases, however, the changes in recertification will lead to eligible beneficiaries who are unable to navigate the bureaucratic tangles to lose health insurance coverage. Losing Medicaid coverage due to procedural or administrative reasons is a common occurrence, and is sure to happen in this seismic transition.
Mitigating the Medicaid Dropoff
States have some options to ease the transition as Medicaid rules change. The Centers for Medicare and Medicaid Services (CMS) has offered strategies states may use. CMS suggests that states pursue renewals with available data whenever possible, rather than reaching out to individual beneficiaries to submit information needed for renewal; expanding use of available data sources (from IRS and state unemployment data to data from other means-tested programs like SNAP) could increase the capacity for renewals. States can also take numerous steps to reduce barriers to eligibility renewal, conducting public outreach and making the process as customer-friendly and streamlined as possible.
The Center on Budget and Policy Priorities encourages state action on the issue. It advocates similar strategies for streamlining the renewal process. States should also plan for the massive increase in workload by staggering renewals so that no individual’s renewal gets lost in the cracks. Similarly, states should consider working to transition those who may lose Medicaid coverage into other health insurance coverage options wherever possible. By planning ahead, Michigan (and other states) can avoid the shock that would come from a sudden mass disenrollment from Medicaid.
Medicaid provided a means to ensure millions of Americans retained healthcare access during the coronavirus pandemic, including hundreds of thousands of Michiganders. As Michigan transitions away from the public health emergency that has characterized the past two years, it is worth considering the value that healthcare provides to individuals on a continuous basis (and not only during a pandemic).
Judging by the available data, the Healthy Michigan Plan continues to pay dividends for Michigan residents, whether or not they are enrolled in the program.

