In a Nutshell
- Insulin is critical for the management of diabetes for a significant portion of almost 1 million Michigan residents affected by the disease, but insulin prices have risen in recent years.
- Capping the price of insulin can help lower the cost of insulin but has limitations.
- While price caps can help lower insulin costs, an alternative approach is direct state involvement in the manufacturing and distribution of insulin, but this is a novel strategy and carries risks.
Introduction
Prescription drugs that are too expensive aren’t just a problem for the patients who need them. Out-of-control drug prices also strain government budgets and drive-up insurance premiums for others. The complexity of healthcare systems and the nation’s approach to pharmaceutical regulation does not lend itself to a single comprehensive solution to high drug prices, but advocates have recently zeroed in on a particular drug, its importance, and its high cost: insulin.
Diabetes and Insulin
Diabetes is a chronic health condition that impacts how the body regulates blood sugar levels. The body requires glucose (sugar) to perform basic functions. When glucose from food enters the bloodstream, the hormone insulin acts as the gatekeeper that helps transfer the glucose in the bloodstream to the body’s cells. For those with diabetes, their bodies either do not produce enough insulin or their cells do not respond to insulin, causing their glucose levels to remain unbalanced. Symptoms of diabetes can include frequent urination, thirst, hunger, weight loss, blurred vision, and numb or tingling hands and feet, among others. Untreated, diabetes can lead to serious health complications, including heart and kidney disease.
According to the American Diabetes Association (ADA), about 29 million people have diagnosed diabetes, including over 900,000 Michigan adults. Many people take insulin to regulate their blood sugar. Nationally, almost 29 percent of those diagnosed with Type I and Type II diabetes use insulin in some capacity. Using this percentage, we can estimate that roughly 260,000 Michigan residents, about 2.5 percent of the state’s population, rely on insulin for diabetes treatment and management.
Like many prescription drugs, insulin is manufactured and distributed through complex supply chains. Wholesalers, pharmacies, and other entities play a role in providing insulin to consumers, and each can complicate the process. The ADA found in a 2017 report that various aspects of the supply chain and pricing mechanisms have contributed to increases in the price of insulin. The average U.S. list price, or Wholesale Acquisition Cost (WAC), of multiple insulin categories per year increased by 15 percent to 17 percent each year from 2012 to 2016 (see chart below). The report mentions the limited number of manufacturers, which reduces competition and minimizes the pressure on manufacturers to set lower prices, as an important factor in the rising costs.
Average Wholesale Acquisition Cost (WAC) for Insulins, by Product Category, 2012–2016.
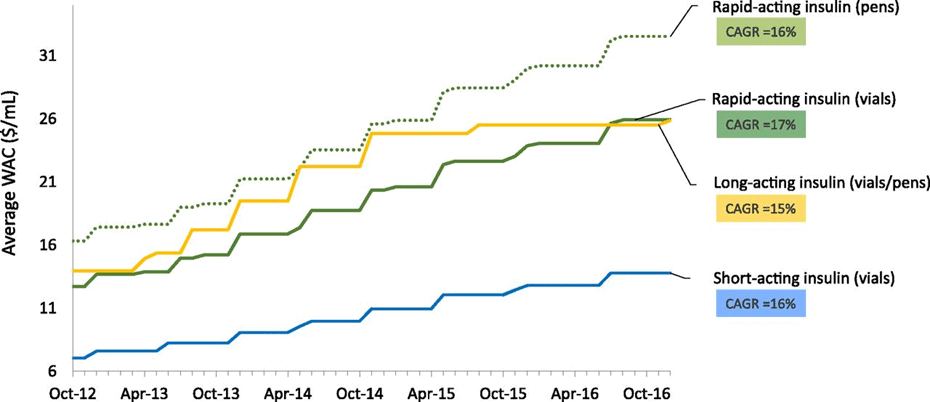
Source: University of Southern California Schaeffer Center analysis of First Databank data.[1] American Diabetes Association. Insulin Access and Affordability Working Group: Conclusions and Recommendations | Diabetes Care | American Diabetes Association (diabetesjournals.org)
Impact of Rising Insulin Prices
It is essential that insulin is affordable to those who need it, and the rise in insulin prices directly impacts the consumer. If the price is unaffordable, those who require insulin may have to sacrifice other basic necessities in order to manage the cost, which could create additional health risks and financial costs. Others may resort to rationing or skipping doses of insulin to cut costs, potentially risking their lives. A study recently published in the Annals of International Medicine found that 16.5 percent of people who use insulin report rationing (about 1.3 million people nationwide). Rates of rationing were higher for middle-income adults, adults under the age of 65, and Black Americans.
The rising cost of insulin impacts more than just the primary consumers. Most states require state-regulated health plans to cover diabetes services, treatments, and supplies, and some states, including Michigan, mandate coverage for both public and private insurers. Higher insulin prices increase costs for health insurance companies, which will likely lead to higher insurance premiums across the board.
Efforts to Reduce Costs
Several potential state and federal policy strategies could reduce the cost of insulin. Some of these strategies focus directly on reducing the price of insulin for consumers, while others target indirect measures to lower costs. Michigan has not taken significant action on these fronts, but policies have been proposed recently that would move Michigan to the forefront of efforts to reduce insulin prices.
To address the cost issue, Michigan’s tax code exempts the “sale of insulin for human use” from state sales and use taxes. Other past initiatives aimed at indirectly reducing the cost of insulin include the Michigan Medicaid Preferred Drug List, a multi-state prescription drug pooling program, and the Pharmaceutical Best Practices Initiative. However, these initiatives can only benefit those who receive insulin through Medicaid.
Price Caps
Enacting an insulin price capis a strategy that has received considerable attention across the country. It aims to reduce the cost of insulin directly for a wider range of consumers. The federal Inflation Reduction Act caps insulin copayments at $35 per month, but only for Medicare patients. Currently, 22 states have enacted laws capping insulin copayments, mostly for state-regulated health plans, with caps ranging from $25 to $100 per month. Several more states have introduced price capping legislation in the past few years. Legislation was introduced in Michigan in 2021 to set the price cap at $50 per month. The bill passed the House but has not been voted on by the Senate.
Price caps have limited efficacy. The cost-savings of price cap legislation may not benefit everyone who requires insulin. For example, while Michigan’s introduced bills would apply to a wide range of health plans, they would not apply to insurance plans that are regulated by the federal government. While the federal government passed an insulin cap for Medicare, the state cap would omit many people who are covered by Medicaid and certain self-insured plans. Similarly, the proposed legislation would not apply to uninsured individuals.
In addition, insulin price caps do not stop manufacturers from raising prices; they merely limit the out-of-pocket co-pays for people who need insulin. This approach ultimately shifts the costs to insurers, which in turn may increase insurance premiums for everyone. This has led some policy strategists to shift the focus of insulin affordability away from price caps and toward the manufacturing process.
State Manufacturing
Earlier this month, Governor Gretchen Whitmer signed an executive directive addressing insulin affordability for Michigan residents. The order instructs state departments and agencies to review aspects of insulin production and identify opportunities to lower costs, including a direct role for the state in the development, manufacturing, and distribution of a low-cost insulin product, with or without outside partners. The directive does not take a firm position on exactly which approach the state should take and leaves it open for departments to consider both public-private partnerships and government-operated manufacturing facilities.
Michigan is not the only state to consider a broader, direct role for the state in manufacturing and distributing insulin. Earlier this year, California included $100 million in its Fiscal 2022-23 state budget for an effort to develop low-cost insulin and set up an in-state manufacturing facility, in partnership with an existing drug manufacturing company.
There is potential value in the state taking a direct role in manufacturing and distributing insulin, particularly in comparison to price caps. Because states do not have regulatory authority over a large share of people covered by health insurance plans that are federally regulated, states are limited in how much they can impact the cost of insulin from insurance-based price caps alone. If the state directly manufactures insulin at a lower cost, however, it can reduce the price paid by individuals who are covered by state-regulated plans and those who are not. Even if the state does not entirely corner the market on insulin sales in the state, the increased competition from state-backed manufacturing activities – which could sell insulin at or below cost – would likely drive down the insulin prices offered by other manufactures.
Direct state investment in manufacturing and distribution would not be without risk. The startup cost for the state would be significant, as indicated by the initial $100 million investment being made in California. A state actually taking on the direct responsibility of manufacturing a prescription medication is a novel policy solution that is not guaranteed to succeed, so it is not certain that this investment will pay dividends. Manufacturing and distributing medication are complex and the feasibility of this approach depends on the state’s ability to provide insulin to the consumer at a lower cost than the existing manufacturers.
While the state has a leg up because it can entirely discount the profit portion of the cost (or even choose to operate at a loss offset by tax revenue), executing an insulin manufacturing operation would require significant expertise and management that cannot be taken for granted. Similarly, it is likely that there would be federal red tape to navigate to ensure that state-produced insulin could make it onto the market. The state has a number of advantages over private manufacturers in terms of price, including the ability to set up the manufacturing sites and distribution network to be optimized for Michigan rather than a national or international system and leveraging the state’s vast purchasing power.
California’s approach to mitigating some of this risk is to partner with an existing drug manufacturer, which is one of the options contemplated by Governor Whitmer’s directive. While a conventional public-private partnership is an option, there are drawbacks. First, any private entity participating in the partnership would seek some level of return on investment which would eat into the potential cost savings. Second, not all drug manufacturers may be eager to join the state’s efforts as the goal of the project – decreasing the price of insulin – would directly affect participating manufacturers’ financial bottom-lines.
It is too early to pass judgement on the feasibility of a particular state-sponsored manufacturing arrangement given that states are just beginning to explore this idea, but policy makers should be taking the concept seriously and investing time and attention toward analyzing how it could be deployed in Michigan.
Conclusion
Rising insulin prices affect a significant portion of residents of every state, including Michigan. While nearly half of the states have instituted some form of co-pay cap on the price of insulin, price caps at the state level only go so far due to the number of plans that are regulated federally. If the state can develop a low-cost approach to manufacturing its own insulin, the upfront cost of building out the infrastructure may be worth it. Not only would it lead to lower insulin prices – which would have direct benefits for people with diabetes – it would likely help attract people to the state through lower health insurance costs and could help demonstrate the state’s ability to leverage its financial resources to solve problems that cannot be solved by markets alone.
[1]Compound Annual Growth Rate is the mean annual growth rate of an investment over a specified period of time longer than one year.

