On January 11th, federal health officials gave the go-ahead for states to experiment with new work requirements in the Medicaid program through Section 1115 demonstrations. This change represents a dramatic shift in federal policy for the 50-year-old Medicaid program (reversing decisions under past Democratic and Republican administrations). Putting aside any discussion regarding the cultural and historical significance of this shift, it seems worth mentioning that most non-elderly, non-disabled adult Medicaid beneficiaries already work or share a household with someone who does. This suggests that the federal policy change may be little more than a favorite old solution in search of a new problem.
In the federal guidance offered to state Medicaid directors, work requirements are promoted as a means to generate better health outcomes based upon numerous statistical associations (e.g., better education is often accompanied by better health and higher earnings are associated with longer lifespan). The guidance also suggests alignment of Medicaid requirements to match the Temporary Assistance for Needy Families (TANF) and Supplemental Nutrition Assistance Program (SNAP) program policies of exempting various populations, such as pregnant women, primary caregivers, students, individuals with disabilities, etc.; however, these suggestions are hardly presented as firm “guardrails” to catch those with the greatest barriers to employment. Moreover, while admonishing states to provide supportive services and workforce training programs to meet employment eligibility, the guidance offers no means for financing such endeavors, clarifying explicitly that “federal Medicaid funding will be limited to allowable activities directly linked to Medicaid beneficiaries.”
Several states have already made requests to include work requirements in their Medicaid programs. Kentucky’s proposal was recently granted approval, and, among Michigan’s neighbors, Indiana and Wisconsin have also made waiver requests. Seven other states (a total of ten) across the country have submitted waiver proposals seeking to add work requirements so far.
In the U.S., there is general belief that people should work for what they get, underscored by the high cultural value placed in ideas of fairness, reciprocity, and self-sufficiency. It’s certainly easy to sympathize with the idea that individuals should do something to earn the increasingly costly health benefits they receive at public expense. In practice, however, numerous challenges and questions surrounding work requirements for a program like Medicaid and this policy change may do more harm than good.
The Heritage Foundation cautions that denying medical care to sick, poor people will be, at minimum, politically and administratively challenging. Moreover, while the policy may reduce Medicaid enrollment by denying coverage to some individuals, it may also increase costs by driving people to emergency rooms rather than encouraging prevention and continuous care. Furthermore, if individuals lose coverage and go without care management, resulting increases in morbidity and/or disability may make them more expensive future beneficiaries when they inevitably sicken to the point to re-qualify without any work requirement. The practical effect of this policy change may be to increase both short-term and long-term costs; any potential savings would be more likely to come from restricting access to needed medical interventions than from any increase in income or self-sufficiency.
Health experts from the Kaiser Family Foundation point out numerous issues surrounding Medicaid work requirements, including administrative burdens, reporting complexities (which can lead to aid being cut to eligible individuals, even when they meet the new requirements), and a shaky theoretical premise. “Robust independent evaluation” of the waivers’ successes or failures in achieving targeted outcomes and their impact on Medicaid beneficiaries are suggested.
The assumption that Medicaid enrollees don’t work (and won’t work unless you threaten to withhold access to medical care) does not align with available evidence. Additional analysis by the Kaiser Family Foundation (see Chart 1) found that most Medicaid beneficiaries already work or else have significant barriers to employment.
Chart 1
Work Status and Reason for Not Working Among Non-SSI, Nonelderly Medicaid Adults, 2016
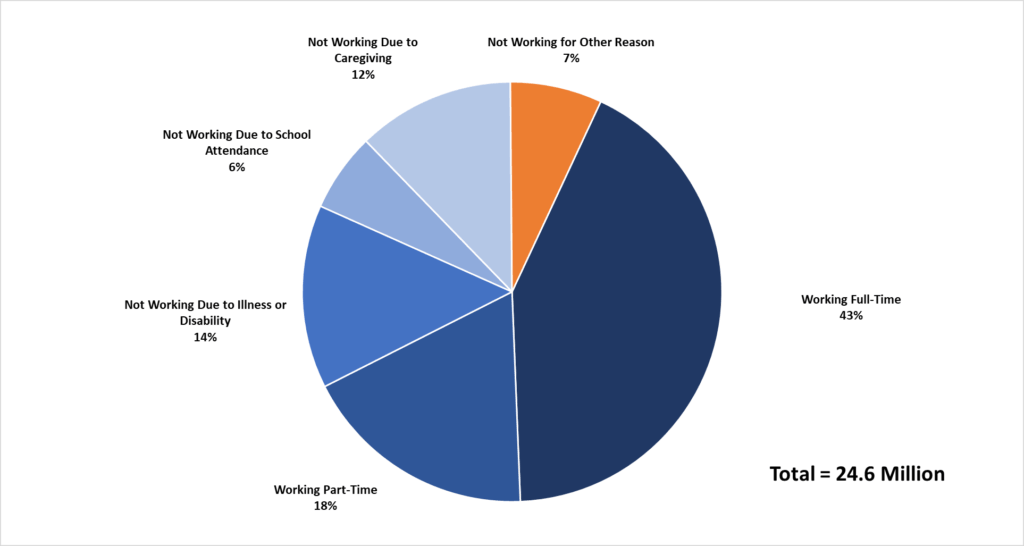
Source: Kaiser Family Foundation
In research on the “Healthy Michigan Plan” expansion of Medicaid last year, the Citizens Research Council noted that the majority of non-disabled adult beneficiaries already work or share a household with someone who does. According to another study in Michigan looking specifically at adults with at least 12 months of coverage through the Healthy Michigan Plan, just over a quarter (27.6 percent, or 104,534 adults) were found to be out of work (see Chart 2); however this group includes a substantial number of individuals who, while not classified as disabled, face many obstacles to employment, like chronic physical and/or mental illness and functional limitations. Among the “out of work” adults in this study, 74 percent had a chronic health condition (65.1 percent had at least one physical health condition, and 35.3 percent had a mental health condition). Additionally, 24.4 percent had a physical functional impairment and 25 percent had a mental functional impairment.
Chart 2
Michigan Medicaid Expansion Enrollee Work Status, 2016
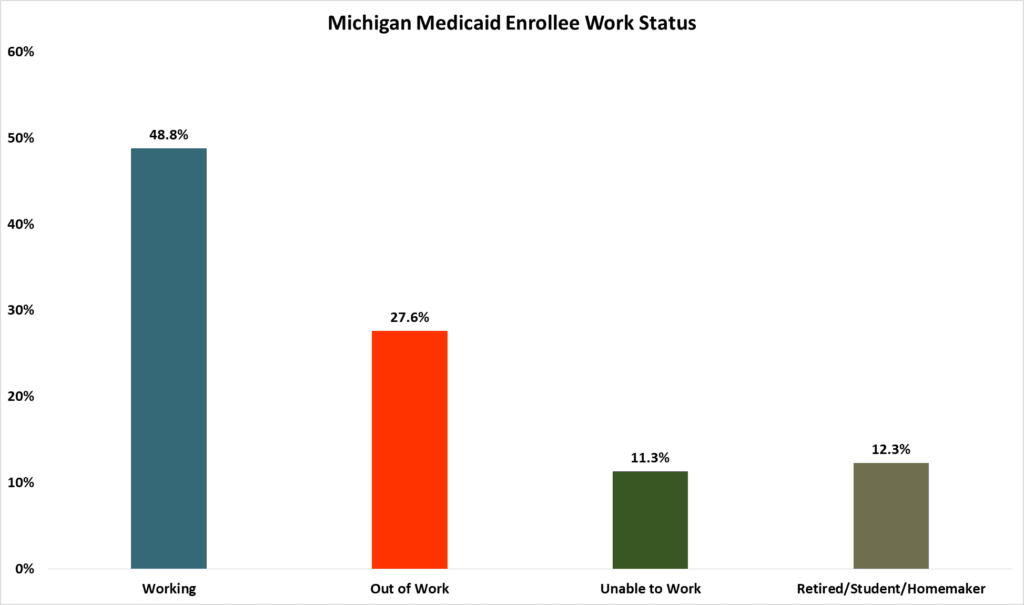
Source: Tipirneni et al., JAMA Internal Medicine
These adults in the expanded Medicaid population are, again, only a fraction of Medicaid recipients (who have traditionally been the disabled, low-income seniors, and, more recently, children). Chart 3 illustrates the proportions of various types of Medicaid coverage. The population targeted by the authorization for states to experiment with work requirements is predominantly represented by the red slice of the pie chart.
Chart 3
Eligible Medicaid Beneficiaries in Michigan by Enrollee Group, December 2016
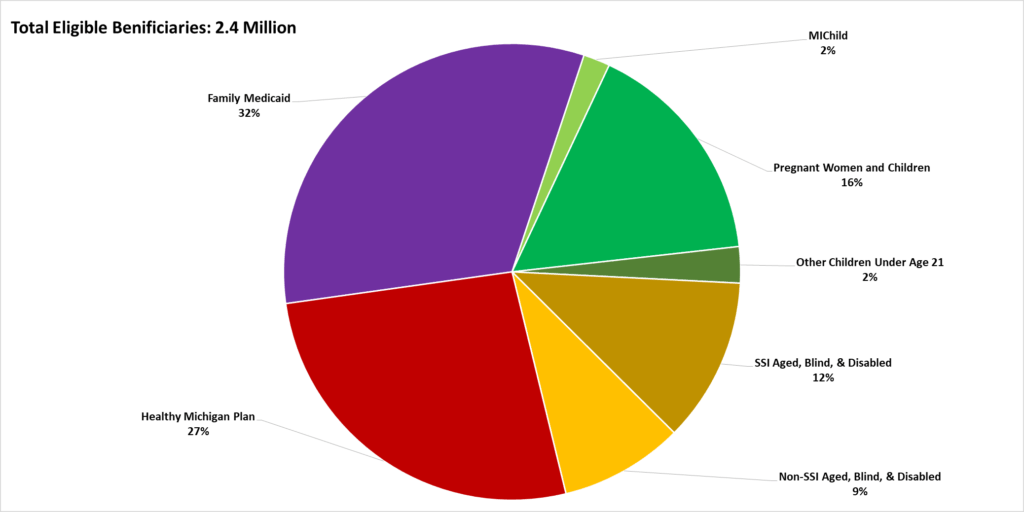
Source: Michigan Department of Health and Human Services
Work requirements for truly able-bodied adults without dependents are aimed at a very narrow slice of the Medicaid pie, and the individuals within this slice may face other barriers to employment beyond the aforementioned health issues—such as low literacy. Finding a job isn’t always a simple feat for people facing financial, educational, and health-related barriers, and these barriers may similarly affect individual capacity for structured volunteering opportunities in lieu of employment. Complex, multidimensional factors contribute to poverty and enhance or diminish an individual’s ability to participate in society through work or community engagement. Approaches that focus on developing individuals’ skills by linking benefits to education and workforce training, rather than simply requiring beneficiaries to find a job, seem to be somewhat more successful.
Research from the University of Michigan found that Medicaid expansion in Michigan helped beneficiaries perform better in existing jobs and in job searches, leading to improved employment prospects and stability by making it easier to seek better jobs. Ohio has had similar successes with Medicaid expansion. These findings undermine the implication that Medicaid work requirements are needed to “improve Medicaid enrollee health and well-being through incentivizing work and community engagement…” as stated by CMS. While the correlations between work, income, education, and health are well-established, it is substantially more difficult to determine directions of causation among these complex associations. Some evidence suggests that Medicaid actually enables work by eliminating health-related barriers to productivity and employment. Framing work as a punitive condition of Medicaid assistance would not only threaten enrollee health, but might also exacerbate social factors that both worsen health and keep people out of the workforce to begin with.
Why support a public policy that is largely disconnected from its stated objectives? Commentary from the Heritage Foundation suggests that work requirements in Medicaid are more symbolic than substantial.
If there is one symbol Americans love more than the aforementioned values of self-sufficiency and reciprocity, it is liberty. Michigan policymakers now have the liberty to experiment with work requirements in the Medicaid program. Central to liberty, however, should be the understanding that permissible and advisable are two very different conditions. In other words: just because you can do it, it doesn’t mean you should.

