- Physical distancing is about more than just health care capacity — public health capacity is an equally important consideration.
- Physical distancing orders are socially and economically unsustainable in the long run; the key to avoiding broad economic shutdowns while still protecting health lies in the public health systems, personnel, and infrastructure that monitor and mitigate the spread of disease.
- Volunteer public health workers utilized to fulfill core governmental responsibilities and functions (such as contact tracing) are to be lauded for their generosity and willingness to serve the public, but the pandemic should be a wake up call for Michigan to start investing in public health and expanding the state’s public health workforce that is committed and accountable to the public.
The Citizens Research Council’s 2018 report warned that Michigan’s disinvestment in public health infrastructure and personnel left the state vulnerable to catastrophes like a pandemic. The impact of that disinvestment has been hard to comprehend in the absence of an event with massive consequences. The Flint water crisis, Hepatitis A outbreak, PFAS contamination, and now the COVID-19 pandemic are making the impact painfully obvious.
Some other governments (e.g., South Korea) were able to mount swift public health responses to the first identified cases of COVID-19 and better mitigate the spread of infection through widespread testing, case identification, contact tracing, and targeted isolation. The United States, however, frankly lacked the capacity to mount similar public health responses, and was eventually forced to implement widespread economic shutdowns and stay at home orders as a last ditch effort to arrest the spread of the novel disease.
Michigan’s “Stay Home, Stay Safe” orders have saved lives and prevented our state’s health care providers from being overwhelmed by cases exceeding capacity. It should be noted, however, that the effort to “flatten the curve” was not solely based on the number of hospital beds or ventilators. On the contrary, physical distancing and other public health recommendations are multifaceted in their purpose and impact.
There Are Many Reasons for Physical Distancing
Nonpharmaceutical interventions (NPIs) like physical distancing have a long history of success at reducing overall attack rates and total deaths from disease during a pandemic. While NPIs provide an added tool alongside medical treatments and vaccines, they also buy time for these pharmaceutical interventions to be developed and refined, and for the understanding of novel pathogens to advance (thereby ideally improving treatment outcomes for people if they become infected later).
While health care capacity is an important consideration, public health capacity deserves equal attention. The moment the SARS-CoV-2 virus was identified, warning bells should have sounded about our (lack of) public health capacity in the face of a probable pandemic. And yet, no discernable public concern was paid to the capacity of our state and local health departments to fight the pandemic in the way health care capacity has been highlighted and discussed.
While newspapers questioned if we had enough physicians, nurses, and hospital beds, few if any asked the same of our epidemiologists, health educators, and other public health practitioners. While we worried about the need for ventilators and PPE for those on the front lines, it seemed little attention was paid to outdated technology and data systems limiting our disease surveillance abilities.
Ironically, attending to these latter public health factors would have done a great deal to alleviate the risk and burden placed on front line health workers and might have reduced the prolonged need for stay-at-home orders.

…But Ongoing Physical Distancing is Socially and Economically Unsustainable
As is obvious from the economic fallout and social unrest, society-wide physical distancing is not sustainable as a long-term pandemic strategy.
And as we recently wrote, it is time to move past narratives that create a false dichotomy out of health and the economy. Economic harms have long been associated with adverse health outcomes. On the other hand, no economy can thrive without healthy people acting as workers and consumers.
Public health experts have known from the start that the only path to keeping the economy open while also keeping a handle on the pandemic lies in robust public health infrastructure, namely disease surveillance, data collection and analysis, and, crucially, contact tracing.
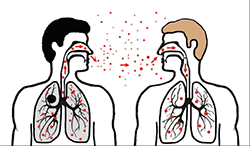
Contact tracing is the long-established process of identifying people who have been exposed to a contagious disease and preventing further spread by tracking down people the exposed person had contact with, to break the chain of transmission. Contact tracers must be equal parts detective, disease expert, and case manager, answering questions about disease symptoms and providing health education while also helping connect people to needed services and supports. Contract tracing has been utilized for decades to address other infectious diseases (e.g., sexually transmitted infections). The techniques of contract tracing, notification, and quarantine are some of the most time-tested public health techniques available, particularly for infectious diseases with no available or proven treatments.
Michigan, with its underfunded public health departments and long-neglected public health infrastructure, comes nowhere near the capacity needed to mount any serious effort.

Michigan Lacks the Capacity for Necessary Public Health Activities
One estimate suggests that a minimum of 30 contact tracers per 100,000 people are needed to handle the current COVID-19 emergency (double the baseline estimate for ongoing public health activities). That means that Michigan needs around 3,000 contact tracers during the pandemic (and a routine, ongoing need for 1,500 contact tracers absent the current pandemic). With a reported 130 state employees designated to do the work, along with a selection of staff from Michigan’s 45 local health departments, Michigan struggles to meet 10 percent of the needed capacity (and that’s while directing staff to COVID-19 and away from other, ongoing health needs).
What is Michigan’s solution to this calamitous lack of preparation, personnel, and infrastructure?
While some may argue that supplementing state capacity with volunteers is the only realistic option to mount any kind of near-term public health response, it’s a less-than-ideal response to our current emergency, and no response at all to our ongoing public health needs as a state.
Michigan’s need for modernized public health systems and a strong public health workforce is apparent, but not new.
Federal appropriations may help. The state has been granted $21.6 million of federal funding thus far to support disease surveillance, infection control, contact tracing, and related public health activities through the March 6th Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020 (P.L. 116-123). CDC initiatives provided additional public health funding for Michigan in the first round of federal stimulus. The third round of stimulus through the CARES Act (P.L. 116-136) means Michigan can count on at least another $16.2 million to support some core public health activities during the pandemic.
The question is: How can Michigan carry this investment beyond the current pandemic response?
The army of retired healthcare providers and graduate students signing up to work through an ongoing pandemic deserve our praise and gratitude; however, Michigan deserves a public health workforce that is professional, highly trained, and fully accountable to the public it serves.
No volunteer corps, however qualified and well-intentioned, can be expected to match the reliability and accountability of a dedicated professional workforce. Similarly, as the Brookings Institution has already written, there are significant problems with the assumption that new applications and technology can take the place of highly trained and educated public health practitioners.
We should not assume that our only problem is getting through the pandemic, after which our public health needs will subside. Bolstering the ranks of Michigan’s public health personnel would give the state valuable epidemiologists, public health analysts, and health educators to deal with the litany of health risks that have affected (and afflicted) Michigan long before the arrival of COVID-19 – risks that will certainly persist after the eventual (with any luck) departure of this devastating (and deadly) disease du jour.

