- While many turn their attention to potential future health reforms, data surrounding the 2014 expansion of insurance coverage under the Affordable Care Act (through new marketplaces and expanded Medicaid) is still being collected and analyzed
- Several states have continued to reject the ACA’s expansion of Medicaid that provides insurance coverage for—and actively improves the health of—adults with very low incomes
- The Citizens Research Council of Michigan was able to share facts from Michigan’s experience with expanding Medicaid—the Healthy Michigan Plan—with policy leaders and analysts from around the country
Last week, I had the honor of presenting my research on Michigan’s expansion of Medicaid to colleagues from around the nation at the Governmental Research Association’s annual conference. The Citizens Research Council benefits greatly from exchanging ideas and experience with like-missioned, non-partisan policy organizations that do similar work in other states and regions.

Since joining the Citizens Research Council, I’ve written quite a bit about the Medicaid program, in particular Michigan’s expansion of Medicaid under the Affordable Care Act: the Healthy Michigan Plan. I’ve blogged about the complicated, arcane challenges involved in funding the state’s share of the Medicaid program.
I’ve also written about continued growth in the Medicaid program as more states adopt expansion, about how Medicaid can play an active role in identifying health risks and improving health, and about how the advent of work requirements for Medicaid enrollees are primarily an ideological solution in search of a problem.They are as likely to imperil health as much as they are to encourage employment by failing to acknowledge the fundamental point that one must be healthy in order to work.
My message to the other researchers was that Michigan offered many lessons, especially for those from states that have not implemented Medicaid expansion.
Michigan’s Experience
Implementation of Healthy Michigan began in April 2014. Due to pent up demand, enrollment surpassed the first-year goal of 322,000 enrollees in just 100 days and has contributed to a large drop in the number of uninsured in Michigan. Today, 660,949 Michiganders receive health insurance through the Healthy Michigan Plan. More than 45 percent of beneficiaries are young (18-34 years of age), and most work in low wage or seasonal jobs that do not provide insurance.
Proportion of the Population Lacking Health Insurance, U.S. and Michigan, 2010-2016
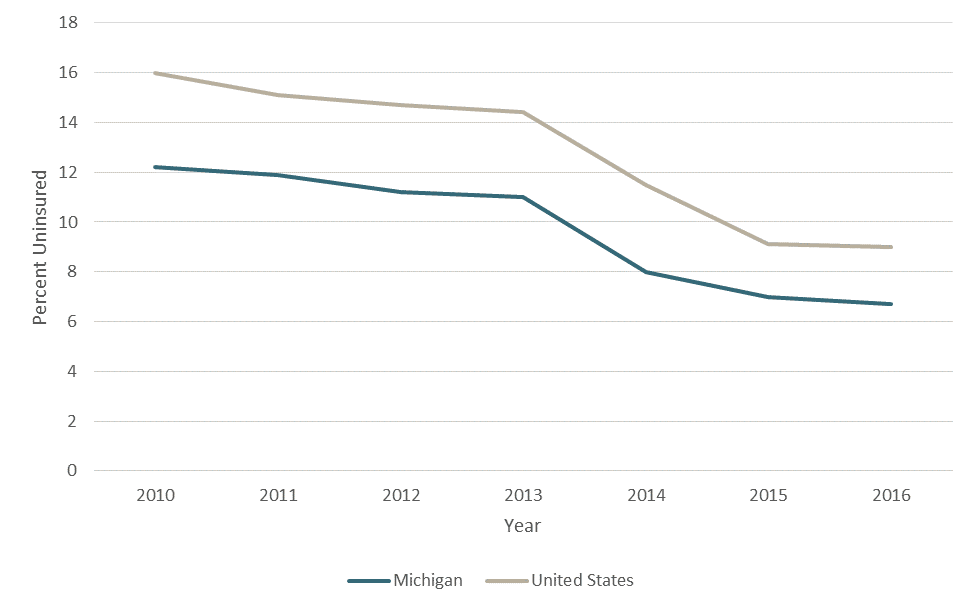
Source: CRC Report #398 ”Medicaid Expansion: Prescription for a Healthier Michigan”
But, beyond these numbers, what has Medicaid expansion meant for health care cost, access, and quality in Michigan?
Medicaid spending constitutes roughly one-third of Michigan’s $57.2 state budget. Of the $19.2 billion dedicated to health care services spending, 71 percent goes toward traditional Medicaid and another 22 percent funds Healthy Michigan. The federal government picks up the majority of these Medicaid costs (70 percent).
Michigan State Budget (in billions), FY2019
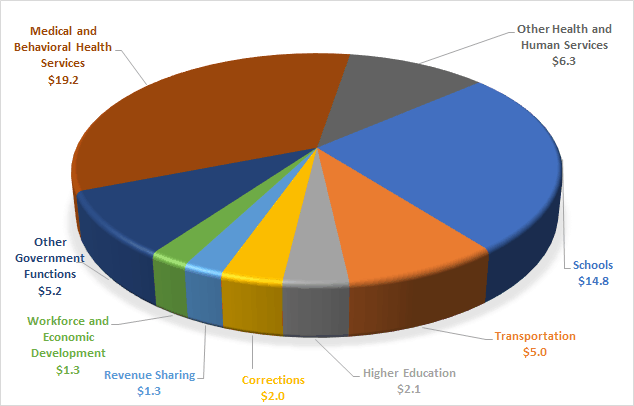
Source: House Fiscal Agency
It might be worth noting that, while senior citizens and persons with disabilities constitute around one in four Medicaid beneficiaries, about two-thirds of the costs are for these populations. Since these individuals generally receive traditional Medicaid benefits, Medicaid expansion is generally much less costly on a per-person basis.
Ultimately, the state’s General Fund pays $3.1 billion of Michigan’s Medicaid bill; however, General Fund spending for Healthy Michigan is just $192 million of this total. Michigan has been very successful leveraging funding from the federal government and other sources to pay for the expanded program.
At its inception, the Healthy Michigan Plan was implanted with a self-destruct device by legislators who were either cost-averse, ideologically opposed, or both. If the net costs of Medicaid expansion to the state exceed savings produced by the expansion, the program will automatically terminate. Thus far, this mechanism shows no signs of triggering. The FY2019 cost of $192 million is offset by $403 million in budget savings in areas such as prisoner health care and mental health services.
State spending is, of course, just one aspect of cost that doesn’t capture the value provided by Medicaid insurance plans. By effectively managing care and preventing overcharging by providers, the per-person cost of Medicaid plans has grown much more slowly than the cost of employer-sponsored health plans during the same period. Moreover, research suggests that people in states that expanded Medicaid pay less for non-Medicaid private health plans as a result (since Medicaid expansion leads to a healthier individual market risk pool and a reduction of bad debt on the part of health providers, among many other factors). As for the beneficiaries, Michigan obtained a federal waiver to include copays and premium contributions for Medicaid enrollees; these costs are capped at a percentage of income and have remained affordable for the people who pay them.
An insurance policy alone doesn’t guarantee access, of course. Medicaid expansion did not have a negative effect on primary care appointment availability for either Medicaid enrollees or people with other private coverage, however, nor did it have a negative effect on appointment availability for new Medicaid patients in Michigan. Access to behavioral health and dental services remains challenging in Michigan and elsewhere. (Moreover, with our maldistribution of health care providers, access in some parts of the state are a challenge no matter the source of insurance). Yet in terms of access, Medicaid beneficiaries fare as well as (and in some cases, better than) people with employer-sponsored health insurance plans.
And what of quality?
Medicaid beneficiaries generally receive high-quality care. In fact, the Healthy Michigan Plan has facilitated health improvement for many enrollees. This improved health facilitates greater workforce participation, better performance at school or work, and greater financial stability. Every person in Michigan enjoys a portion of these benefits, whether or not people are themselves enrolled in Medicaid; indeed, the economic benefits that the state has enjoyed from Medicaid expansion have been tremendous.
The Response from Other Policy Experts
Shawn Teigan, vice-president and research director at Utah Foundation, noted that our analysis from Michigan provided a wealth of information. He recounted how Utah’s legislature had initially resisted Medicaid expansion before slowly moving to adopt a modest, scaled-back expansion of the program; Utah voters, however, took to the issue to the ballot and voted in favor of full expansion—an expansion that the legislature has subsequently scaled back once again to resemble its initial proposal.
Jason Stein, Research Director at the Wisconsin Policy Forum, discussed how Wisconsin has a traditional Medicaid program with more expansive coverage than most states, but that the Affordable Care Act’s expansion of Medicaid was resisted by the state (Wisconsin is the only state in the Great Lakes Region that has not expanded its Medicaid program). He pointed to conflicting projections made by different studies surrounding Medicaid expansion and highlighted the need for high-quality, unbiased facts and data. In this regard, we were happy to oblige insofar as Michigan’s experience can inform policymakers from other states.
The Healthy Michigan Plan is arguably one of Michigan’s greatest bipartisan achievements to come out of Lansing in recent years. In 2017, our report on Medicaid expansion found that the program was largely a success story; 18 months later, that analysis has been reaffirmed by updated data.

